Fatty liver while pregnant is a rare but serious condition that affects some women during pregnancy. The liver plays a vital role in keeping the body healthy, and during pregnancy, it undergoes extra strain due to the demands of the growing baby. Fatty liver during pregnancy, also known as Acute Fatty Liver of Pregnancy (AFLP), occurs when fat builds up in the liver cells, disrupting the organ’s function.
If left untreated, this condition can lead to severe complications for both the mother and the baby. The key to managing fatty liver while pregnant is understanding the symptoms, risk factors, and treatments available. Early detection and intervention are essential for a safe pregnancy and a healthy baby.
What is Acute Fatty Liver of Pregnancy (AFLP)?
Acute Fatty Liver of Pregnancy (AFLP) is a rare but potentially life-threatening liver disorder that typically occurs in the third trimester of pregnancy. It is characterized by the accumulation of fat in the liver cells, which disrupts the liver’s ability to function properly. Although it is uncommon, affecting approximately 1 in 10,000 to 15,000 pregnancies, AFLP is a serious condition that requires immediate medical attention.
The exact cause of AFLP is not entirely understood, but it is often associated with metabolic changes in the mother during pregnancy. If left untreated, fatty liver while pregnant can lead to liver failure, kidney failure, and even death. However, with early detection and proper management, most women recover fully after delivery.
Signs and Symptoms
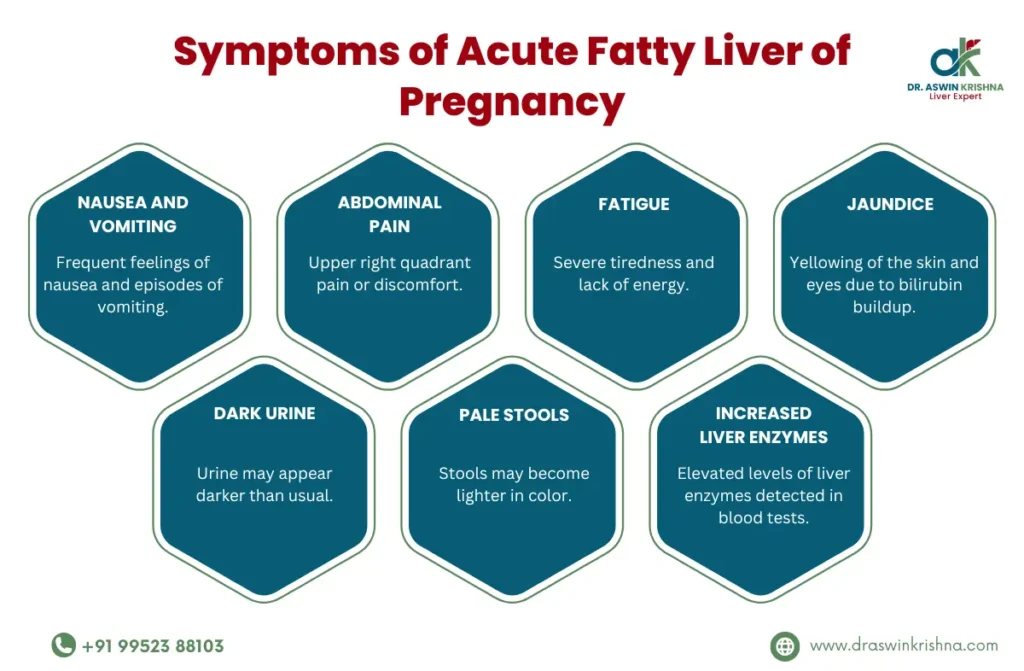
The symptoms of acute fatty liver of pregnancy can be varied and may resemble other common pregnancy-related conditions, making it difficult to diagnose without thorough testing. Symptoms usually begin in the third trimester and can escalate quickly. Here are the most common signs and symptoms to look out for:
- Nausea and vomiting
- Abdominal pain, especially in the upper right side
- Fatigue and weakness
- Jaundice (yellowing of the skin and eyes)
- Swelling in the legs, feet, and hands
- Severe headaches
- Confusion or mental disorientation
- Rapid weight gain due to fluid retention
These symptoms can easily be mistaken for other issues like preeclampsia or gallbladder problems, so it’s crucial to get medical advice if they appear, especially if they worsen quickly.
Causes
The exact cause of acute fatty liver of pregnancy remains unclear. However, some theories suggest that it may be related to metabolic changes that occur inflamed liver during pregnancy. One known contributing factor is a genetic deficiency in the enzymes responsible for breaking down fatty acids in the liver. When these enzymes do not work properly, fat accumulates in the liver, leading to inflammation and liver damage.
Other factors may include hormonal changes, increased liver stress during pregnancy, and pre-existing liver conditions that can be exacerbated by pregnancy. While the precise cause is not fully known, it is clear that fatty liver while pregnant is a condition that needs immediate medical attention once it is detected.
Risk Factors
Several factors can increase a woman’s risk of developing fatty liver while pregnant. Though this condition is rare, understanding the risk factors can help in early detection and prevention. Some of the most common risk factors for AFLP include:
- First pregnancy – Women in their first pregnancy are more likely to experience AFLP.
- Carrying multiples (twins or triplets) – Having more than one baby increases the chances of developing the condition.
- Pre-existing liver conditions – Women with a history of liver problems may be at higher risk.
- Obesity or being overweight – Excess weight can increase the strain on the enlarged liver during pregnancy.
- Family history of liver disorders – A genetic predisposition may increase the risk of AFLP.
If you fall into any of these categories, it’s important to inform your doctor so they can closely monitor your liver health throughout pregnancy. Early detection is key to preventing complications.
Complications
If not diagnosed and treated promptly, fatty liver while pregnant can lead to several severe complications. Some of these complications may pose life-threatening risks to both the mother and the baby. Common complications of AFLP include:
- Liver failure – As fat builds up in the liver, it can stop functioning properly.
- Kidney failure – AFLP can also affect the kidneys, leading to kidney failure if untreated.
- Severe bleeding – AFLP can interfere with the blood’s ability to clot, which can cause dangerous bleeding.
- Premature birth – Many women with AFLP require early delivery, which can increase the risk of complications for the baby.
- Stillbirth – In severe cases, AFLP can result in stillbirth if not diagnosed early.
These complications highlight the importance of liver support during pregnancy. Working closely with your healthcare provider to monitor your liver function test and overall health is essential to avoiding these risks.
Diagnosis
Diagnosing acute fatty liver of pregnancy can be challenging due to its similarities with other pregnancy-related conditions. To confirm the diagnosis, doctors will perform a variety of tests, including:
- Blood tests – These can check for elevated liver enzymes, which indicate liver stress or damage.
- Imaging tests – Ultrasound or MRI scans can help detect an enlarged liver during pregnancy and assess the extent of fat accumulation.
- Liver biopsy – In rare cases, a biopsy may be needed to confirm the diagnosis. This involves taking a small sample of liver tissue for examination.
Given the potential complications, early diagnosis is crucial. If a fatty liver while pregnant is suspected, medical teams will often recommend close monitoring and may prepare for early delivery to reduce the risks.
Treatment for Fatty Liver While Pregnant
If AFLP is diagnosed, the primary treatment is usually the immediate delivery of the baby, as this is the most effective way to stop the progression of the disease. In most cases, symptoms of fatty liver while pregnant improve after delivery. Additional treatments may include:
- Hospitalization – Close monitoring and supportive care are often required.
- Intravenous fluids – These help maintain hydration and support liver function.
- Medications – Some women may need medications to manage symptoms or complications, like blood clotting issues.
- Blood transfusions – If severe bleeding occurs, blood transfusions may be necessary.
Recovery from AFLP can take time, and liver function should continue to be monitored after delivery to ensure there is no lasting damage.
Prevention
There is no guaranteed way to prevent fatty liver while pregnant, but there are steps you can take to reduce your risk. These include:
- Regular prenatal check-ups – Consistent monitoring can help catch any signs of liver issues early.
- Maintaining a healthy weight – Managing your weight before and during pregnancy can reduce the strain on your liver.
- Managing pre-existing conditions – If you have a history of liver disease, work with your healthcare provider to monitor your liver throughout the pregnancy.
- Balanced diet – Eating a diet rich in fruits, vegetables, and whole grains can support overall liver health and reduce the risk of fatty liver.
These prevention methods can significantly lower the chances of developing complications related to fatty liver while pregnant.

When Should I See My Healthcare Provider?
Seek immediate medical attention if you experience symptoms of Fatty Liver While Pregnant. These may include:
- Persistent nausea and vomiting
- Severe abdominal pain, particularly in the upper-right region
- Jaundice (yellowing of the skin and eyes)
- Fatigue and general malaise
- Sudden weight loss or a significant decrease in appetite
Early diagnosis and timely intervention are crucial for managing AFLP. If you have a history of liver issues or a genetic predisposition, regular check-ups are vital. Your healthcare provider may recommend blood tests, liver function panels, or ultrasound imaging to monitor your liver health.
Key Points About Acute Fatty Liver of Pregnancy
- Rare but Serious Condition: AFLP affects approximately 1 in 10,000 to 15,000 pregnancies.
- Causes: The exact cause is unknown, but genetic factors and mitochondrial dysfunction may contribute.
- Symptoms Develop Quickly: Unlike other liver conditions, AFLP can progress rapidly in the third trimester.
- Diagnostic Tests: Blood tests show elevated liver enzymes, low blood sugar, and signs of kidney dysfunction.
- Treatment Involves Delivery: Immediate delivery is the only effective treatment once AFLP is diagnosed.
- Recovery: Post-delivery, liver function typically returns to normal with proper medical care.
- Follow-up is Essential: Future pregnancies may carry a higher risk; consult your doctor for tailored liver support during pregnancy.
Conclusion
Fatty liver while pregnant is a rare but potentially life-threatening condition that requires immediate attention. Understanding the symptoms, risk factors, and treatment options can help you stay proactive in managing your health liver support during pregnancy. With regular check-ups, early detection, and proper medical care, the risks associated with inflamed liver during pregnancy can be minimized, ensuring a safe and healthy pregnancy for both mother and baby.



