Cirrhosis, a chronic and progressive liver condition, significantly impairs the organ’s ability to perform essential tasks like detoxification and nutrient metabolism. For patients with end-stage cirrhosis, a liver transplant is often the only pathway to recovery. This advanced surgical procedure replaces a diseased liver with a healthy donor organ, enabling patients to regain their health and vitality. Understanding the causes, symptoms, and transformative benefits of a liver transplant for cirrhosis can help patients and their families make empowered decisions.
What is Cirrhosis?
Cirrhosis occurs when prolonged damage to the liver results in the formation of scar tissue, which disrupts normal liver functions. This scarring develops over time, leading to severe complications that can be life-threatening without intervention.
Major Causes of Cirrhosis
- Chronic Alcohol Abuse: Regular and excessive alcohol consumption is a leading cause of liver damage.
- Hepatitis Infections: Persistent inflammation from viral infections like hepatitis B, hepatitis C, or D accelerates liver scarring.
- Nonalcoholic Fatty Liver Disease (NAFLD): Linked to conditions such as obesity, high cholesterol, and Type 2 diabetes.
- Hereditary Disorders: Genetic conditions, including Wilson’s disease and hemochromatosis, can trigger cirrhosis.
Recognizing and addressing these causes early can slow disease progression and improve patient outcomes.
What is a Liver Transplant for Cirrhosis?
A partial liver transplant for cirrhosis is a highly specialized surgical procedure where a diseased liver is replaced with a healthy one from a donor. For advanced cirrhosis, it is often the only effective treatment to restore the liver’s essential functions.
Types of Liver Transplants
- Deceased Donor Transplant: A full liver from a deceased donor is used to replace the damaged organ.
- Living Donor Transplant: A portion of the liver is transplanted from a living donor. The liver’s ability to regenerate makes this a viable option.
Dr. Aswin Krishna offers both types of transplantation, tailoring the approach to each patient’s unique medical needs.
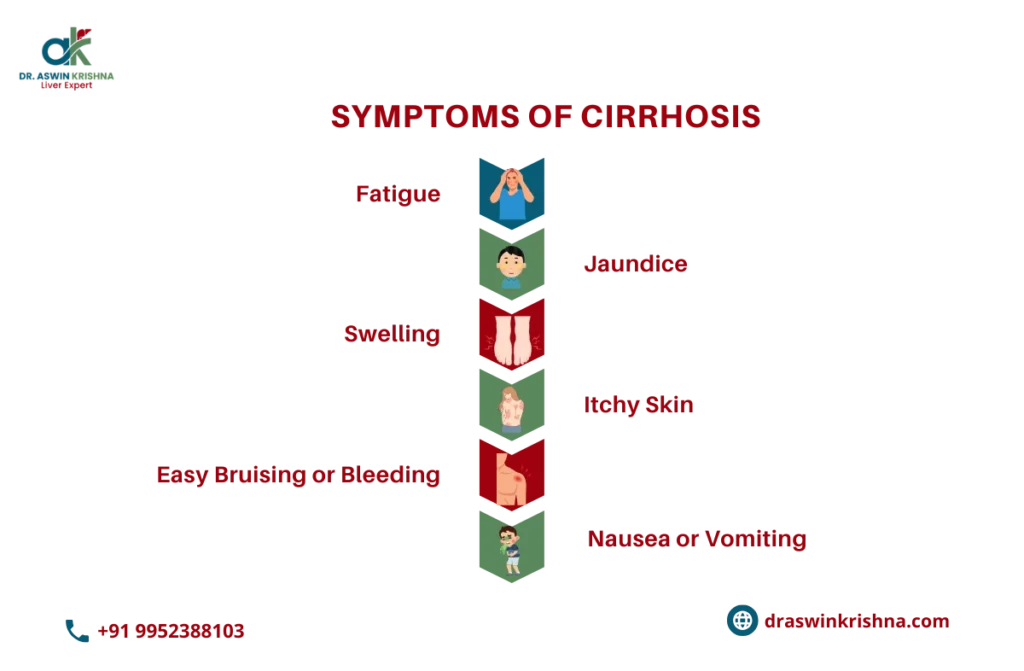
Symptoms of Advanced Cirrhosis
Cirrhosis develops gradually, often remaining undetected until signs of cirrhosis have occurred.
Common Symptoms
- Chronic Fatigue: Persistent tiredness and lack of energy.
- Yellowing of the Skin and Eyes (Jaundice): Caused by an accumulation of bilirubin.
- Abdominal Swelling (Ascites): Fluid buildup in the abdomen.
- Loss of Appetite: Leading to unintended weight loss.
- Itching and Bruising: Resulting from reduced liver function.
- Mental Confusion: Toxin buildup in the blood can affect brain function.
These symptoms and signs of cirrhosis indicate severe liver damage and necessitate immediate medical attention to explore options like a partial liver transplant for cirrhosis.
Complications of Untreated Cirrhosis
Without timely treatment, cirrhosis can lead to serious health issues that drastically reduce life expectancy.
Key Complications Include:
- Liver Failure: When the liver can no longer perform basic functions like detoxification or protein synthesis.
- Internal Bleeding: High blood pressure in the veins surrounding the liver causes life-threatening hemorrhages.
- Kidney Impairment: Cirrhosis of the liver can lead to renal dysfunction due to systemic complications.
- Liver Cancer: The likelihood of developing liver cancer increases significantly with advanced cirrhosis.
A partial liver transplant for cirrhosis can prevent these complications, offering a chance to reclaim health and quality of life.
Prevention of Liver Transplantation for Cirrhosis
Preventing the need for a Liver Transplant for Cirrhosis begins with early intervention, lifestyle modifications, and regular monitoring of liver health. The focus is on controlling the underlying causes of liver damage to halt or slow the progression of fibrosis before it reaches an irreversible stage.
- Avoiding Alcohol and Toxins: For those with alcoholic liver disease, complete abstinence from alcohol is critical. Continuous alcohol intake accelerates liver scarring, often making liver transplant for alcoholic cirrhosis inevitable.
- Managing Hepatitis Infections: Timely treatment of hepatitis B and C through antiviral medications helps prevent cirrhosis progression and may eliminate the need for liver transplant for non alcoholic cirrhosis.
- Healthy Diet and Weight Control: Obesity and fatty liver disease increase cirrhosis risk. Maintaining a balanced diet rich in antioxidants, fiber, and lean proteins supports liver regeneration and reduces inflammation.
- Regular Health Checkups: Early detection through imaging and liver function tests allows doctors to manage cirrhosis effectively before reaching the liver transplant criteria for cirrhosis stage.
Stages of Liver Transplantation for Cirrhosis
The Liver Transplant for Cirrhosis process occurs in multiple phases, from evaluation to post-transplant recovery. Each stage ensures patient safety and maximizes the likelihood of successful liver regeneration.
- Pre-Transplant Evaluation: Comprehensive tests assess liver function, overall health, and psychological readiness. This stage helps determine the indications for liver transplant in cirrhosis, identifying those most likely to benefit.
- Donor Selection: Depending on the severity and urgency, doctors may recommend a living donor liver transplant for cirrhosis or a partial liver transplant for cirrhosis, where a section of a healthy liver is used for transplantation.
- Transplant Surgery: The diseased liver is removed, and the donor liver (whole or partial) is connected to the recipient’s blood vessels and bile ducts.
- Post-Transplant Recovery: Lifelong follow-up care and immunosuppressive medications are necessary to prevent rejection and ensure the new liver functions efficiently.
Benefits of Liver Transplantation for Cirrhosis
A Liver Transplant for Cirrhosis offers renewed life quality and improved long-term survival for patients in advanced disease stages.
- Restoration of Liver Function: The new liver efficiently performs detoxification, protein synthesis, and bile production, reversing complications caused by cirrhosis.
- Improved Quality of Life: After a successful living donor liver transplant for cirrhosis, patients experience reduced fatigue, enhanced appetite, and improved mental alertness.
- Long-Term Survival: Advances in surgical techniques and immunotherapy have increased survival rates, particularly in liver transplant for alcoholic cirrhosis and liver transplant for non alcoholic cirrhosis cases.
- Reduced Risk of Complications: It eliminates symptoms like portal hypertension, variceal bleeding, and ascites, allowing patients to live healthier lives.
How Liver Cirrhosis Affects Overall Health
Cirrhosis affects nearly every system in the body by impairing the liver’s vital roles in metabolism, detoxification, and nutrient storage.
- Digestive and Nutritional Impact: The liver’s inability to process nutrients leads to malnutrition, vitamin deficiencies, and muscle wasting.
- Hormonal and Immune Dysfunction: Cirrhosis disrupts hormonal balance and weakens immunity, making patients prone to infections and metabolic disorders.
- Neurological Complications: Accumulation of toxins like ammonia causes hepatic encephalopathy, leading to confusion, memory loss, and cognitive decline.
- Cardiovascular and Renal Effects: Severe cases can cause portal hypertension and hepatorenal syndrome, emphasizing the urgency for Liver Transplant for Cirrhosis.
The Role of Liver Transplant in End-Stage Cirrhosis
For patients with end-stage liver disease, Liver Transplant for Cirrhosis is often the only definitive treatment.
- Replacement of Irreversibly Damaged Tissue: The transplant substitutes the scarred liver with a healthy one, restoring essential physiological functions.
- Extending Life Expectancy: It significantly improves survival rates, especially in those meeting the liver transplant criteria for cirrhosis after medical therapy failure.
- Applicable to Different Causes: Whether due to hepatitis, alcohol, or metabolic diseases, both liver transplant for alcoholic cirrhosis and liver transplant for non alcoholic cirrhosis have demonstrated excellent post-surgery outcomes.
When is Liver Transplantation Necessary for Cirrhosis Patients?
Determining the indications for liver transplant in cirrhosis depends on the stage of liver failure and symptom severity.
- Advanced Liver Dysfunction: Transplantation becomes necessary when jaundice, ascites, or hepatic encephalopathy persist despite medical therapy.
- Complications of Portal Hypertension: Frequent variceal bleeding and refractory ascites are key signs that the patient has reached liver transplant criteria for cirrhosis.
- Poor Quality of Life: When cirrhosis limits physical activity or causes recurrent infections, a living donor liver transplant for cirrhosis may be considered to improve survival and comfort.
How Liver Transplant Restores Liver Function in Cirrhosis
The ultimate goal of a Liver Transplant for Cirrhosis is to replace the diseased organ with a healthy one capable of performing normal metabolic activities.
- Restoration of Detoxification and Metabolism: The new liver eliminates toxins and processes nutrients effectively, alleviating symptoms like fatigue and confusion.
- Regeneration and Growth: In partial liver transplant for cirrhosis, the transplanted liver segment regenerates rapidly, achieving full functionality within weeks.
- Enhanced Longevity and Stability: Patients receiving liver transplant for alcoholic cirrhosis or liver transplant for non alcoholic cirrhosis often enjoy decades of improved liver function and overall health.
- Sustained Organ Function: With proper post-transplant care and medications, the new liver maintains balance across digestive, immune, and hormonal systems, promoting lasting wellness.
Criteria for Liver Transplant in Cirrhosis
Not everyone with cirrhosis is eligible for a liver transplant. Here are the primary criteria considered:
- Severity of Liver Disease: The Model for End-Stage Liver Disease (MELD) score determines the urgency of a transplant. A higher score indicates a more severe condition.
- Underlying Cause of Cirrhosis: Common causes include chronic hepatitis, alcohol-related liver disease, non-alcoholic fatty liver disease (NAFLD), and autoimmune conditions.
- Overall Health: Patients should not have uncontrolled infections, active cancer outside the liver, or severe heart/lung disease.
- Commitment to Lifestyle Changes: Candidates must commit to abstaining from alcohol and maintaining a healthy lifestyle post-transplant.
- Psychological Readiness: Mental health evaluations ensure that patients are emotionally prepared for surgery and post-operative care.
Conclusion
A liver transplant for cirrhosis is a transformative treatment for those battling the challenges of advanced cirrhosis. By replacing the diseased liver with a healthy one, this procedure offers renewed hope, improved quality of life, and extended longevity. Dr. Aswin Krishna specializes in providing tailored liver transplant solutions, guiding patients through every step of the process to ensure optimal outcomes. If you or someone you love is facing advanced liver disease, seek expert advice today to explore the possibilities of a brighter tomorrow.




