The liver transplant process is a vital medical procedure offering hope to individuals with severe liver conditions. This intricate surgery involves several carefully planned steps, from selecting a suitable donor to implanting a healthy liver and ensuring its proper function. Each phase plays a crucial role in restoring the patient’s health and quality of life. With expert care and precision, the process can be life-saving, offering patients a second chance to lead a healthier life.
The Liver Transplant Process
Donor Liver Procurement
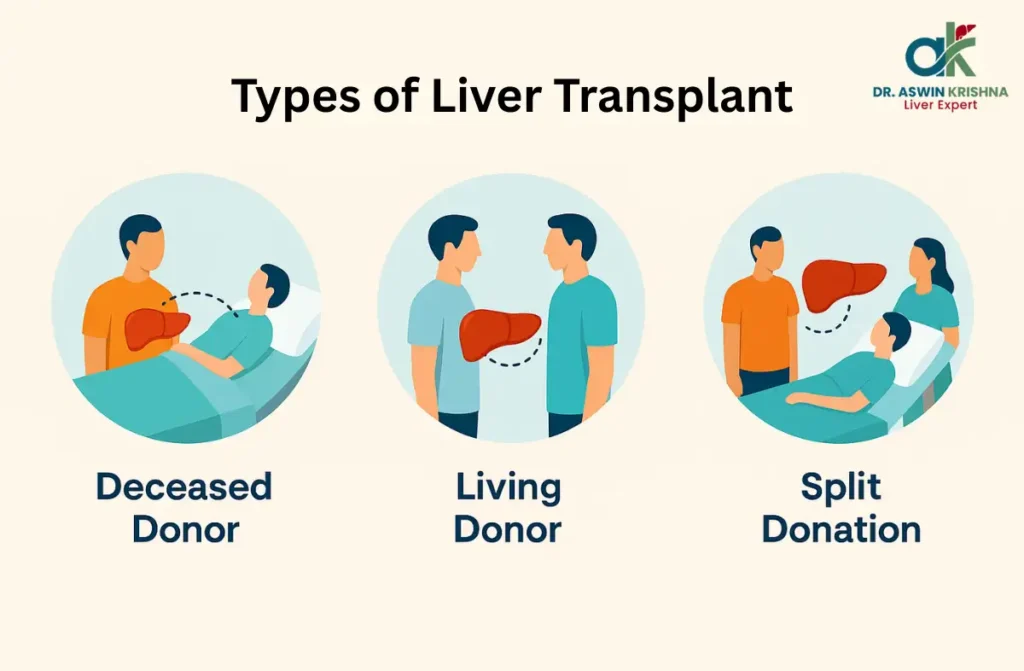
The first step in the liver transplant process is securing a healthy and compatible donor liver. This can be from either a living donor or a deceased donor, depending on the situation and urgency. Finding the right match is critical to avoid complications and ensure a successful transplant.
Key aspects of donor liver procurement:
- Living Donor: A close family member or a willing individual donates a part of their liver, which regenerates over time.
- Deceased Donor: Livers are retrieved from brain-dead individuals after obtaining consent from their families.
- Rigorous tests are conducted to confirm organ transplant process compatibility.
This step ensures the recipient receives a liver capable of restoring their health.
Recipient Preparation
Preparing the patient for the liver transplant process is a critical phase that ensures their body is ready to receive the donor liver. This step involves thorough medical evaluations and stabilization to minimize potential complications during surgery.
Key steps include:
- Comprehensive health assessments: Blood tests, imaging, and organ function evaluations.
- Stabilizing the patient’s condition to optimize surgical outcomes.
- Immunosuppressive medications planned to prevent organ rejection after surgery.
This stage ensures the patient is in the best possible health for the procedure, making the liver transplant procedure in India a safe and effective solution for end-stage liver disease.
Anesthesia and Incision
The liver transplant process begins with administering general anesthesia, ensuring the patient remains unconscious and free of pain throughout the surgery. Once the patient is anesthetized, the surgeon makes a carefully planned incision in the upper abdomen to access the liver.
Key aspects of this stage include:
- General anesthesia ensures complete comfort and safety.
- A precise incision minimizes post-surgical scarring and promotes healing.
- Advanced techniques are used to reduce surgical risks.
This step is essential in creating a safe environment for the subsequent procedures, ensuring the patient is stable during the liver transplant surgery time of 6–12 hours.
Hepatectomy (Removal of Diseased Liver)
The hepatectomy phase in the liver transplant process involves removing the diseased liver to prepare for the implantation of the donor liver. This step requires precision to ensure the safety and readiness of the patient’s body for the new organ transplant process.
- The surgeon carefully detaches the liver from major blood vessels.
- Any surrounding tissues are examined and preserved as needed.
- Care is taken to avoid unnecessary bleeding or trauma.
This step is critical in the liver transplant surgery time, as it sets the foundation for the successful implantation of the donor liver.
Implantation of Donor Liver
The liver transplant process reaches a critical phase with the implantation of the donor liver. The healthy liver, either from a living or deceased donor, is carefully positioned into the recipient’s abdominal cavity. This stage demands precision to ensure proper alignment and minimize complications.
Key steps include:
- Placing the donor liver securely in the recipient’s body.
- Ensuring it fits anatomically with minimal tension on surrounding structures.
- Preparing for vascular and bile duct connections.
During the liver transplant surgery time, surgeons meticulously check for stability before moving to the next phase, ensuring the procedure’s success.
Vascular Anastomosis
Vascular anastomosis is a critical step in the liver transplant process that ensures proper blood flow to the newly transplanted liver. Surgeons reconnect the recipient’s major blood vessels to those of the donor liver, creating a seamless circulatory system essential for liver function. This phase requires precision and expertise to avoid complications and ensure the liver receives adequate oxygen and nutrients.
Key steps in vascular anastomosis:
- Connection of the hepatic artery to provide oxygen-rich blood.
- Attachment of the portal vein for nutrient supply.
- Reconnection of the inferior vena cava to drain deoxygenated blood.
This meticulous process ensures the transplanted liver integrates successfully with the body.
Bile Duct Reconstruction
The final step in the liver transplant process is bile duct reconstruction, a critical phase to ensure proper bile flow from the liver to the digestive system. This step plays a vital role in restoring normal digestion and liver function.
Key elements of bile duct reconstruction:
- Connecting the donor bile duct to the recipient’s bile duct or intestine.
- Ensuring a leak-proof connection to prevent complications.
- Using advanced surgical techniques to minimize risks.
Proper bile duct alignment ensures efficient bile transportation, reducing the risk of post-surgery complications. This step completes the liver transplant procedure in India, ensuring the patient’s smooth recovery.
Candidates for Liver Transplant
- Who qualifies for a transplant: The liver transplant process is generally considered for individuals with irreversible liver failure, certain cases of liver cancer, or acute liver damage that cannot be treated by other means. Doctors assess whether the surgery can improve life expectancy and quality of life before moving forward.
- Medical and health factors: Candidates must have advanced liver disease severe enough to outweigh the risks of major surgery. The evaluation includes checking other vital organs like the heart and kidneys to ensure the body can handle the procedure. This step is a vital part of the liver transplant process.
- Age and overall fitness: While there is no strict Maximum age for liver transplant, biological health plays a bigger role than the number of years lived. Frailty, heart health, and other medical issues are considered to determine suitability.
- Special circumstances: People with liver cancer meeting strict criteria, metabolic disorders, or acute liver failure may be fast-tracked in the liver transplant process. In cirrhosis cases, the Criteria for liver transplant in cirrhosis focus on symptoms like repeated bleeding, fluid buildup, or cancer within transplantable limits.
Health Screening Before Transplant
- Laboratory tests: Candidates undergo liver function tests, kidney function checks, clotting profiles, and screenings for viral infections such as hepatitis. These results help calculate disease severity and determine urgency within the liver transplant process.
- Heart and lung assessments: Tests like ECG, echocardiograms, and lung function exams check if the patient can safely undergo surgery. In many cases, these assessments influence the decision regarding the Maximum age for liver transplant by revealing fitness levels.
- Lifestyle and support evaluation: Patients are screened for mental readiness, social support, and ability to follow long-term medication schedules. Good support systems are crucial for post-surgery success.
- Cirrhosis-specific criteria: The Criteria for liver transplant in cirrhosis include decompensated symptoms such as persistent fluid buildup, repeated bleeding episodes, and certain liver cancers. These guidelines ensure organs go to patients who will benefit most.
Surgery Process
- Step-by-step procedure: The liver transplant process involves removing the damaged liver and replacing it with a healthy donor liver. Blood vessels and bile ducts are reconnected to restore normal function.
- Time required for surgery: A typical liver transplant surgery time ranges from six to twelve hours, depending on the patient’s condition and surgical complexity. In some rare cases, it can take longer.
- Living donor vs. deceased donor operations: Living donor transplants involve transplanting a portion of the liver and can require simultaneous surgeries for donor and recipient. This may affect the liver transplant surgery time due to added preparation steps.
- Long-term success: Many patients live decades after surgery, with the Longest liver transplant survivor living over 40 years. These outcomes are possible due to medical advancements and careful post-surgical care.
Post-Surgery Follow-Up Care
- Hospital recovery: After the operation, patients usually spend several days in intensive care for close monitoring of organ function, wound healing, and possible complications. This early stage is crucial in the liver transplant process.
- Medication management: Long-term use of immunosuppressants prevents organ rejection. These drugs must be taken exactly as prescribed to avoid complications and maintain the transplanted liver.
- Ongoing monitoring: Regular check-ups involve blood tests, imaging scans, and health reviews to ensure the liver is functioning well. This structured follow-up is key to long-term success.
- Exceptional outcomes: While many recipients live well beyond a decade, some, like the Longest liver transplant survivor, show that multi-decade survival is possible with consistent care.
Diagnostics for Liver Transplant
- Imaging and scans: CT and MRI scans check the liver’s condition, blood vessel structure, and tumor presence. These are vital for surgical planning in the liver transplant process.
- Blood and functional tests: Frequent lab tests measure liver enzymes, clotting ability, and kidney function to track disease progression and readiness for surgery.
- Cancer and infection checks: For patients with cirrhosis, tests help confirm eligibility according to the Criteria for liver transplant in cirrhosis. Screening also detects infections that must be treated before surgery.
- Whole-body assessment: Heart, lung, dental, and psychological evaluations ensure the patient is fully prepared for surgery and the demanding recovery that follows.
Candidates for Liver Transplant
Not everyone with liver disease is a candidate for a transplant. Doctors evaluate several factors before recommending this life-saving procedure. You might be considered for the liver transplant process if you suffer from:
- Chronic Liver Diseases: Conditions like liver cirrhosis, hepatitis B and hepatitis C, or non-alcoholic fatty liver disease.
- Liver Cancer: Early-stage hepatocellular carcinoma confined to the liver.
- Acute Liver Failure: Sudden, severe liver malfunction caused by infections, drug reactions, or toxins.
- Inherited Liver Conditions: Genetic diseases like hemochromatosis or Wilson’s disease.
Patients undergo a thorough evaluation, including physical exams, imaging tests, and psychological assessments, to determine if they are fit for the liver transplant procedure in India.
Delaying Liver Transplant and Prolonging Life
While a transplant might seem urgent, certain lifestyle changes and medical treatments can delay the need for surgery and help prolong life:
- Medication Management: Following prescribed medications to manage symptoms and slow disease progression.
- Healthy Diet: A liver-friendly diet low in fats and high in fiber supports overall liver health.
- Avoiding Alcohol and Toxins: Abstaining from alcohol and limiting exposure to harmful substances can reduce liver stress.
- Regular Monitoring: Regular medical check-ups ensure early detection of complications.
Delaying the transplant doesn’t mean ignoring symptoms; instead, it focuses on managing the disease effectively until the liver transplant process becomes necessary.
Liver Transplant Surgery Time
The liver transplant surgery time typically ranges from 6 to 12 hours, depending on the complexity of the procedure and the patient’s condition. The steps include:
- Preparation: Administering anesthesia and preparing the patient for surgery.
- Removal of the Diseased Liver: Carefully detaching the damaged liver from surrounding tissues.
- Implantation of the Donor Liver: Connecting the new liver to blood vessels and bile ducts.
- Post-Surgery Monitoring: Ensuring the body accepts the new liver without complications.
After the surgery, patients stay in the intensive care unit (ICU) for close observation, followed by a longer recovery period in the hospital.
Conclusion
The liver transplant process is a transformative procedure that provides new hope to patients with end-stage liver disease. From donor selection to bile duct reconstruction, every step is meticulously planned to ensure successful outcomes and restore health. By addressing the complexities with precision and care, this process offers a second chance at life. For expert guidance and comprehensive care, trust Dr. Aswin Krishna to support you through every stage of this life-saving journey.




