Stage 5 liver failure is a life-threatening condition that marks the end of a progressive decline in liver function. By the time someone reaches this stage, the liver has sustained irreversible damage, often leading to liver cancer. In this blog post, we’ll explore what stage 5 liver failure entails, the different stages leading up to it, its causes, and possible treatments. Understanding this progression is crucial to early intervention and prevention, making a significant difference in a patient’s quality of life.
Types
There are two primary types of liver failure: acute and chronic.
- Acute Liver Failure: This type of liver failure develops rapidly, often within days or weeks. It’s usually caused by factors like drug overdose (especially acetaminophen), viral infections, or toxins. Although acute liver failure can occur in individuals with no prior history of liver disease, it is an emergency condition requiring immediate medical intervention.
- Chronic Liver Failure: Chronic liver failure, on the other hand, occurs gradually over months or years. It is typically the result of prolonged liver damage due to conditions like hepatitis, long-term alcohol abuse, or fatty liver disease. Over time, the liver becomes increasingly scarred and loses its ability to regenerate, leading to chronic liver failure, which can culminate in stage 5 liver damage.
Causes
Liver failure occurs when large portions of the liver become damaged beyond repair, preventing it from functioning properly. The most common causes include:
- Chronic Alcohol Abuse: Long-term alcohol consumption leads to liver inflammation and scarring, eventually causing cirrhosis and liver failure.
- Hepatitis B and C: Viral hepatitis is a significant cause of liver inflammation, which can develop into chronic liver disease and lead to liver cancer.
- Fatty Liver Disease: Obesity, poor diet, and metabolic disorders contribute to the accumulation of fat in the liver, leading to non-alcoholic fatty liver disease (NAFLD), which can progress to cirrhosis and liver failure.
- Autoimmune Diseases: Conditions like autoimmune hepatitis cause the body’s immune system to attack liver cells, causing inflammation and damage.
- Genetic Disorders: Diseases such as Wilson’s disease and hemochromatosis can cause an accumulation of toxic substances in the liver, damaging its cells.
All these factors contribute to a gradual decline in liver function, eventually leading to stage 5 liver disease, where cancer can form.
Symptoms
Liver disease symptoms often progress silently until advanced stages like stage 5 liver disease. Common symptoms include:
- Persistent fatigue and weakness.
- Yellowing of the skin and eyes (jaundice).
- Abdominal swelling and pain due to fluid retention (ascites).
- Dark urine and pale stools.
- Unexplained bruising or bleeding.
- Loss of appetite, nausea, or vomiting.
- Cognitive issues like confusion, memory loss, or difficulty concentrating.
Stages of Liver Disease
Liver disease can develop over time, and the condition worsens in five distinct stages. Each stage has its own set of symptoms and treatment options, with Stage 5 being the final and most severe. The stages include:
- Stage 1: Inflammation
- Stage 2: Scarring
- Stage 3: Cirrhosis of the Liver
- Stage 4: End-stage Liver Disease (ESLD)
- Stage 5: Liver Cancer
As the liver progresses through these stages, the damage becomes increasingly difficult to reverse, and the chances of recovery diminish. Let’s take a closer look at each stage.
Stage 1: Inflammation
In the earliest stage of liver disease, inflammation occurs as the liver responds to injury or infection. Common causes include hepatitis viruses, alcohol abuse, fatty liver disease, or autoimmune conditions. Inflammation often presents no symptoms, though fatigue or abdominal discomfort can occur. If left untreated, this condition worsens and progresses to scarring. Fortunately, lifestyle changes, such as quitting alcohol or managing infections, can reverse liver inflammation. Early intervention plays a crucial role in halting the disease’s progression and preventing future complications, ensuring that the liver can continue to function properly for years to come.
Stage 2: Scarring
Also known as fibrosis, Stage 2 liver disease involves the formation of scar tissue, which begins to replace healthy liver cells. This scarring happens as a result of untreated inflammation and reduces the liver’s ability to function efficiently. Symptoms are typically mild or nonexistent but may include fatigue and slight abdominal pain. Though scarring at this stage is still reversible, early detection is vital. Lifestyle changes, medications, and addressing the underlying causes of liver damage can slow progression. If ignored, fibrosis can worsen, leading to irreversible damage and eventually advancing to cirrhosis in the next stage.
Stage 3: Cirrhosis of the Liver
In Stage 3 liver disease, extensive scarring leads to cirrhosis, where the liver’s ability to regenerate is severely compromised. The organ becomes stiff, impairing blood flow and liver function. Symptoms often include jaundice (yellowing of the skin), fatigue, swelling in the legs or abdomen, and confusion due to toxin buildup. At this stage, treatment focuses on managing complications and slowing progression through medications, lifestyle changes, and regular monitoring. Cirrhosis increases the risk of developing liver cancer and may require a liver transplant if the damage becomes life-threatening. Early medical intervention can help improve long-term outcomes.
Stage 4: End-stage Liver Disease (ESLD)
End-stage liver disease (ESLD) occurs when liver function declines drastically, leaving the body unable to detoxify blood, process nutrients, or produce essential proteins. Symptoms include severe jaundice, persistent fluid buildup, gastrointestinal bleeding, and mental confusion due to hepatic encephalopathy. Without a liver transplant, survival rates are low. Treatment at this stage focuses on managing symptoms, preventing infections, and improving quality of life. ESLD is often a consequence of untreated cirrhosis or liver failure and marks a turning point where immediate medical intervention is necessary to prolong life and ease the suffering of affected individuals.
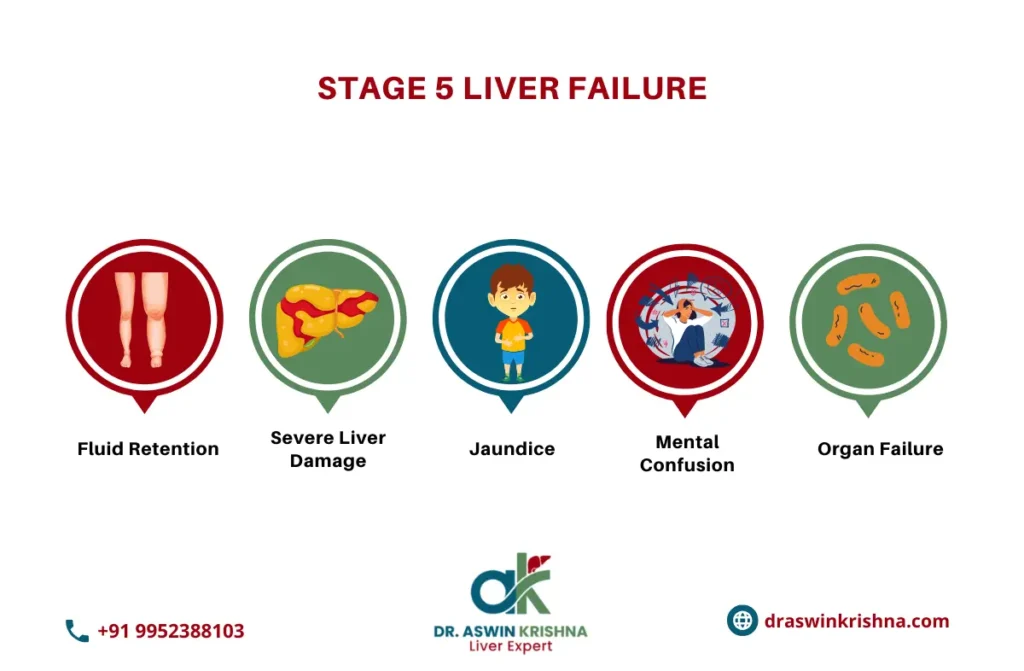
Stage 5: Liver Cancer
In the final and most severe stage, stage 5 liver cancer develops as a result of prolonged liver damage, usually caused by cirrhosis or hepatitis. At this point, the liver has sustained irreversible damage, and cancerous cells begin to spread. Symptoms include unexplained weight loss, persistent upper abdominal pain, fatigue, and jaundice. Treatment options depend on the cancer’s stage and can include chemotherapy, targeted therapies, or liver transplantation. Unfortunately, the prognosis for stage 5 liver disease is often poor, making early detection of earlier stages crucial. Palliative care becomes essential to maintain comfort and quality of life.
Liver Disease and Liver Failure Diagnosis
The liver, a vital organ, performs critical functions such as detoxification, protein synthesis, and bile production. In stage 5 liver failure—the most severe stage—liver function deteriorates to the point of life-threatening consequences. Diagnosis often involves:
- Blood tests (Liver Function Tests – LFTs) to assess enzyme and protein levels.
- Imaging studies like ultrasound, CT scan, or MRI for liver damage evaluation.
- Liver biopsy to confirm conditions such as stage 5 liver cancer or cirrhosis.
- Advanced screening for complications like hepatic encephalopathy or portal hypertension.
Treatment
Treatment for liver failure depends on the stage of the disease. Early stages can be managed through:
- Medications: To manage symptoms and treat underlying conditions like hepatitis.
- Lifestyle changes: Avoiding alcohol, eating a liver-friendly diet, and managing other risk factors like obesity.
- Liver transplant: In stage 5 liver damage, a liver transplant is often the only way to survive. It replaces the damaged liver with a healthy donor liver.
Complications
Complications of liver failure can be severe and life-threatening, particularly in stage 5 liver disease. These complications include:
- Internal bleeding: Caused by high blood pressure in the liver’s veins.
- Hepatic encephalopathy: A brain disorder caused by the buildup of toxins in the bloodstream.
- Kidney failure: Often occurs in conjunction with liver failure.
- Infections: Due to a weakened immune system and liver dysfunction.
These complications highlight the importance of preventing liver failure before it progresses to the later stages.
Prevention
The best way to prevent stage 5 liver disease is by taking care of your liver early. Here are some steps you can take:
- Limit alcohol consumption: Excessive alcohol is a major cause of liver disease.
- Maintain a healthy diet and weight: Avoid fatty foods and aim to exercise regularly.
- Vaccinations: Get vaccinated against hepatitis B to reduce the risk of infection.
- Avoid risky behaviors: Like sharing needles or unsafe sexual practices that increase the risk of hepatitis.
- Regular check-ups: Early detection of liver disease can stop it from progressing.
How Long Can You Live With Chronic Liver Failure and End-Stage Liver Disease?
The life expectancy for individuals with stage 5 liver disease depends on multiple factors, including the severity of complications, access to medical care, and whether a liver transplant is an option.
- Without a Liver Transplant: Patients with end-stage liver disease who do not undergo a transplant typically survive 6 months to 2 years, depending on the severity of symptoms and overall health condition.
- With a Liver Transplant: Those who receive a successful transplant have a 5-year survival rate of approximately 75%, with many living for decades with proper post-transplant care.
How Fast Does Liver Disease Progress?
The progression of liver disease depends on its underlying cause and how it is managed. In many cases, chronic liver diseases, such as hepatitis or alcohol-induced liver damage, take years or even decades to reach stage 5 liver disease. Conversely, acute liver failure, caused by infections, toxins, or overdose, can escalate within days or weeks.
Factors Affecting the Speed of Progression:
- Cause of Liver Damage: Chronic diseases (e.g., hepatitis B or C) progress slower than acute conditions.
- Lifestyle Choices: Alcohol consumption and poor diet can accelerate liver damage.
- Medical Interventions: Early detection and treatment can delay or halt disease progression.
- Comorbidities: Diabetes, obesity, or cardiovascular diseases exacerbate liver damage.
Monitoring liver health regularly and adhering to medical advice can significantly slow the progression of liver disease, even in its early stages.
What Does Liver Pain Feel Like?
Liver pain, commonly felt in the upper right abdomen, varies in intensity and sensation. In stage 5 liver damage, it can manifest as:
- A dull, persistent ache or throbbing discomfort.
- Sharp stabbing pain during movement or after meals.
- Pressure-like sensation due to an enlarged liver.
- Radiating pain toward the back or right shoulder blade.
Conclusion
Stage 5 liver failure is the culmination of years of liver damage, often resulting in liver cancer and the need for a transplant. Understanding the 5 stages of liver disease, from inflammation to cirrhosis and beyond, can help individuals recognize symptoms early and take steps toward prevention and treatment. If you’re at risk of liver disease, don’t wait—seek medical attention before it’s too late and prevent reaching stage 5 liver failure.



