Liver fibrosis is a gradual process in which healthy liver tissue is replaced by scar tissue, disrupting the organ’s ability to function properly. Often developing silently over years, this condition is a warning signal of ongoing liver damage caused by infections, alcohol use, or metabolic disorders. Early detection and proper Liver Fibrosis Treatment can halt or even reverse its progression, restoring liver health. Understanding how fibrosis begins and how it can be managed is the first step toward healing and prevention.
What are the Causes of Liver Fibrosis?
Liver fibrosis develops when the liver’s natural healing process is overwhelmed by persistent injury or inflammation. Over time, this leads to the accumulation of scar tissue that impairs liver function. Understanding the liver fibrosis causes is crucial for determining the right Liver Fibrosis Treatment and preventing further damage.
- Chronic Viral Infections: Long-term hepatitis B and C infections are among the leading liver fibrosis causes. These viruses trigger ongoing inflammation that stimulates the liver to produce excess collagen, forming fibrous tissue and replacing healthy cells over time.
- Alcohol-Induced Liver Injury: Continuous alcohol consumption puts immense strain on the liver, leading to inflammation and fat buildup. When this damage becomes chronic, scar tissue develops, making early intervention and Liver Fibrosis Treatment essential to prevent irreversible liver failure.
- Non-Alcoholic Fatty Liver Disease (NAFLD): People with obesity, diabetes, or high cholesterol may develop fatty deposits in the liver even without alcohol consumption. This condition, known as NAFLD, can advance into inflammation and scarring, known as non-alcoholic steatohepatitis (NASH).
- Autoimmune Hepatitis: In autoimmune hepatitis, the body’s immune system mistakenly attacks liver cells, resulting in continuous inflammation. Without timely treatment, this immune-driven injury can lead to progressive fibrosis and loss of liver function.
- Toxin and Drug Exposure: Certain industrial chemicals, environmental toxins, or prolonged use of medications such as methotrexate can damage liver cells. Repeated exposure accelerates fibrotic changes, underscoring the importance of identifying and removing the source.
- Genetic and Metabolic Disorders: Conditions like hemochromatosis (iron overload) and Wilson’s disease (copper accumulation) cause toxic buildups in the liver. These inherited disorders, if untreated, can result in severe scarring and the need for aggressive Liver Fibrosis Treatment to restore balance.
Symptoms of Liver Fibrosis
Liver fibrosis often develops quietly, showing little to no signs in its early stages. As the condition progresses, however, the damage becomes more noticeable through physical and metabolic changes. Recognizing fatty liver fibrosis symptoms early can lead to timely Liver Fibrosis Treatment and prevent progression to cirrhosis or liver failure.
- Persistent Fatigue and Weakness: One of the earliest fatty liver fibrosis symptoms is a constant feeling of tiredness. As the liver struggles to process toxins and store energy efficiently, individuals may experience chronic weakness, reduced stamina, and brain fog.
- Abdominal Pain and Fullness: A dull, persistent ache in the upper right side of the abdomen is common. This discomfort arises from liver swelling and stretching of the capsule surrounding it, indicating ongoing inflammation that requires medical evaluation and Liver Fibrosis Treatment.
- Loss of Appetite and Weight Changes: People may notice unexplained loss of appetite or sudden weight fluctuations. The liver’s reduced ability to digest and store nutrients affects metabolism, leading to nutritional deficiencies and gradual weight loss.
- Jaundice (Yellowing of Skin and Eyes): As fibrosis worsens, the liver’s ability to filter bilirubin diminishes. This buildup leads to jaundice, a clear sign that scarring has advanced and immediate medical attention is required.
- Swelling in Legs and Abdomen (Edema and Ascites): Reduced liver function causes fluid retention in the lower limbs or abdomen. These symptoms often reflect significant progression and should prompt evaluation for advanced Liver Fibrosis Treatment strategies.
- Itchy Skin and Dark Urine: Toxin accumulation in the bloodstream due to poor liver filtration can cause persistent itching and changes in urine color. These signs often appear in moderate to severe stages of fibrosis, signaling liver distress.
Staging of Liver Fibrosis
The severity of liver fibrosis is assessed through specific grading systems that measure how much scar tissue has replaced healthy liver cells. Understanding liver fibrosis stages helps doctors tailor the right Liver Fibrosis Treatment plan, monitor disease progression, and predict long-term outcomes.
- Stage F0 – No Fibrosis: At this stage, the liver is healthy with no visible scarring. Although no Liver Fibrosis Treatment is required, maintaining a balanced lifestyle and avoiding alcohol or viral infections is essential for prevention.
- Stage F1 – Mild Fibrosis: Minimal scarring begins to appear in the liver’s portal areas. Early detection at this level allows for lifestyle adjustments, antiviral therapies, or dietary changes to reverse damage and halt progression.
- Stage F2 – Moderate Fibrosis: Fibrous tissue starts spreading between blood vessels and liver cells, interfering with normal circulation. At this stage, consistent monitoring and medical therapy become necessary to prevent advancement to more severe liver fibrosis stages.
- Stage F3 – Advanced Fibrosis: Scar tissue bridges between different parts of the liver, distorting its structure. Individuals may begin experiencing symptoms like fatigue and abdominal discomfort, and more intensive Liver Fibrosis Treatment is needed to manage inflammation and prevent cirrhosis.
- Stage F4 – Cirrhosis: This is the most severe among the liver fibrosis stages, where extensive scarring leads to permanent liver damage. The liver becomes shrunken and nodular, and complications like fluid buildup or jaundice may occur. Treatment focuses on managing symptoms, preventing further deterioration, and in some cases, evaluating eligibility for liver transplantation.
Complications of Liver Fibrosis
As liver fibrosis progresses, scar tissue begins to disrupt blood flow and essential liver functions. Without timely Liver Fibrosis Treatment, these changes can trigger severe complications that affect multiple organs and overall health. Understanding these risks helps patients and caregivers recognize why early management is vital when asking, “is liver fibrosis curable” or “can liver fibrosis be reversed.”
- Progression to Cirrhosis: The most serious complication of untreated fibrosis is cirrhosis. In this stage, scar tissue replaces most of the healthy liver cells, permanently impairing liver function. Managing fibrosis early is key to preventing this irreversible transformation.
- Portal Hypertension: Scarred liver tissue restricts blood flow through the portal vein, causing increased pressure in the portal circulation. This leads to enlarged veins in the esophagus and stomach, which may rupture and result in life-threatening bleeding if not properly managed with advanced Liver Fibrosis Treatment.
- Ascites and Edema: Fluid accumulation in the abdomen (ascites) and legs (edema) occurs when the liver loses its ability to regulate fluid balance. These complications often indicate late-stage fibrosis, where management focuses on controlling symptoms and improving comfort.
- Hepatic Encephalopathy: When toxins build up in the bloodstream due to poor filtration, brain function becomes affected. Symptoms include confusion, personality changes, and difficulty concentrating, showing how deeply liver dysfunction can influence mental health.
- Liver Cancer (Hepatocellular Carcinoma): Chronic inflammation and scarring increase the risk of liver cancer. Patients with long-standing fibrosis or cirrhosis require regular screening to detect cancer early and begin aggressive Liver Fibrosis Treatment or targeted therapies.
- Liver Failure: In advanced stages, the liver can no longer perform vital metabolic, detoxifying, and storage functions. This condition is life-threatening and may necessitate a liver transplant. However, early intervention can prevent the disease from reaching this critical stage, answering the concern—can liver fibrosis be reversed—with cautious optimism when addressed promptly.
Diagnosis of Liver Fibrosis
Accurate diagnosis of liver fibrosis is essential to determine its extent and to plan an effective Liver Fibrosis Treatment strategy. Since early fibrosis often presents no symptoms, medical evaluation relies on a combination of blood tests, imaging, and specialized procedures. The emergence of new treatment for liver fibrosis has also been supported by advancements in precise diagnostic methods.
- Blood Tests and Liver Function Panels: Routine blood tests measure enzymes such as ALT, AST, and bilirubin, which indicate liver cell injury. Additional tests like the Fibrosis-4 (FIB-4) index and AST to Platelet Ratio Index (APRI) are used to estimate fibrosis levels non-invasively, aiding early treatment planning.
- Imaging Techniques (Ultrasound, FibroScan, MRI): Ultrasound scans can reveal changes in liver texture and stiffness, while FibroScan uses elastography to measure how stiff the liver tissue has become — a strong indicator of scarring. MRI elastography provides even greater detail, allowing doctors to track fibrosis progression and guide Liver Fibrosis Treatment more accurately.
- Liver Biopsy: Still considered the gold standard for diagnosis, a liver biopsy involves extracting a small tissue sample for microscopic analysis. This test provides a precise picture of inflammation and scarring but is usually recommended when imaging results are inconclusive.
- Serological Markers and Advanced Biomarkers: Research into new treatment for liver fibrosis has introduced advanced biomarkers like hyaluronic acid, procollagen III peptide, and TIMP-1, which help assess fibrosis severity without invasive procedures. These evolving diagnostic tools allow for earlier intervention and personalized care.
- Genetic and Metabolic Testing: In cases of hereditary or metabolic liver diseases, specific genetic panels help identify underlying causes such as hemochromatosis or Wilson’s disease. Detecting these conditions early can lead to targeted treatments that prevent further fibrosis progression.
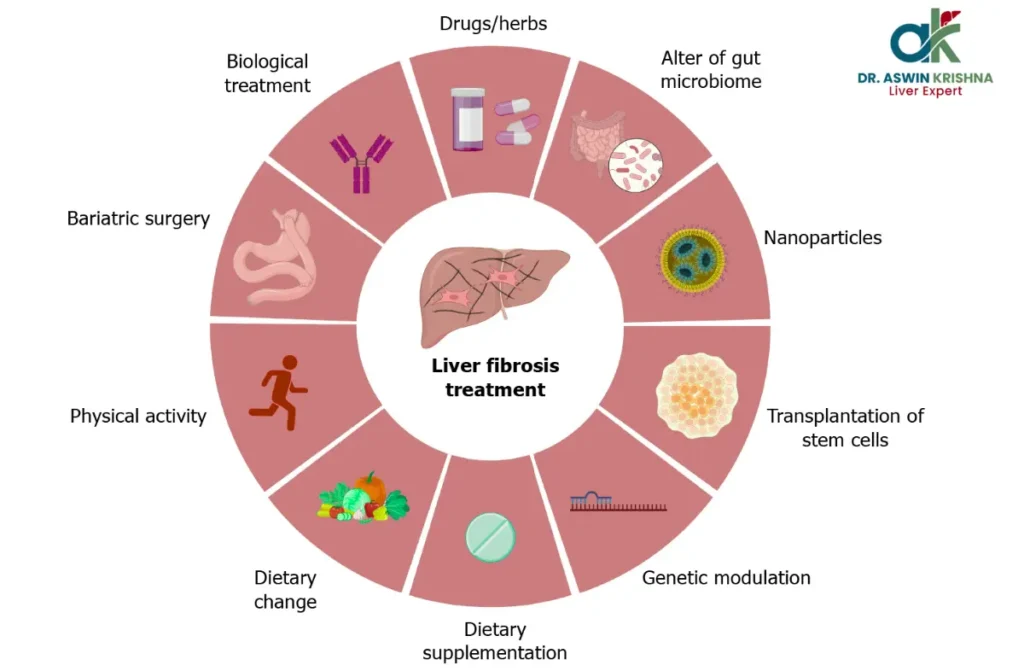
Treatment Options for Liver Fibrosis
Effective Liver Fibrosis Treatment focuses on stopping liver damage, promoting regeneration, and addressing the root cause of scarring. While many ask, “is liver fibrosis curable” or “can liver fibrosis be reversed,” the answer depends on early detection, commitment to lifestyle changes, and adherence to medical guidance. Modern therapies and research into new treatment for liver fibrosis have brought renewed hope for recovery.
- Lifestyle Modifications: The foundation of Liver Fibrosis Treatment begins with eliminating harmful habits. Avoiding alcohol, maintaining a balanced diet rich in antioxidants, exercising regularly, and managing blood sugar and cholesterol levels can significantly reduce inflammation and help the liver repair itself. These steps are vital when understanding how to reverse liver fibrosis naturally.
- Medication for Underlying Causes: The most effective medicine for liver fibrosis targets its source. Antiviral drugs are prescribed for hepatitis B or C, while autoimmune hepatitis may require corticosteroids or immunosuppressants. For fatty liver-related fibrosis, insulin-sensitizing agents and lipid-lowering medications help control disease progression.
- Anti-Fibrotic and Regenerative Therapies: Recent research in new treatment for liver fibrosis includes anti-fibrotic agents that block collagen formation and stimulate liver regeneration. Drugs like obeticholic acid, simtuzumab, and other investigational molecules show promise in slowing or reversing fibrosis in clinical trials.
- Nutritional Support and Supplements: A nutrient-dense diet supports liver healing. Vitamins E and D, omega-3 fatty acids, and antioxidants like silymarin from milk thistle have shown potential in protecting liver cells. A physician can tailor nutritional therapy as part of a broader Liver Fibrosis Treatment plan.
- Management of Complications: If fibrosis has advanced, treatment includes managing portal hypertension, controlling fluid retention, and preventing infections. In some cases, endoscopic or pharmacological interventions are used to prevent internal bleeding caused by varices.
- Liver Transplantation: In cases where the liver is severely damaged, transplantation becomes the only viable option. While it doesn’t reverse existing scarring, it restores liver function completely, offering a new beginning for those whose condition has progressed beyond reversal.
- Emerging Regenerative Medicine: Scientists are exploring stem cell therapy and gene-based new treatment for liver fibrosis to regenerate damaged tissue. These treatments aim not just to manage fibrosis but to restore healthy liver architecture, offering hope that one day can liver fibrosis be cured will have a definitive “yes.”
Conclusion
Liver fibrosis is not the end of liver health—it’s a warning sign that healing must begin. With the right Liver Fibrosis Treatment, early detection, and a commitment to lifestyle changes, the liver has a remarkable ability to regenerate. Whether caused by viral infections, fatty liver, or toxins, taking action at the right time can prevent irreversible damage and restore vitality. Empower your liver, protect your health, and take the first step toward a stronger, healthier future.



